THOUSANDS of pre-school children in Africa could benefit from access to treatment for snail fever, after tests showed infants to be at high risk of infection.
Researchers tested hundreds of children aged between one and five in countries in sub-Saharan Africa where the endemic disease – also known as bilharzia or schistosomiasis – is endemic.
Currently, infants are not regularly tested for infection as they are perceived to be at low risk of exposure to the water-borne disease and not to suffer severely from its ill-effects.
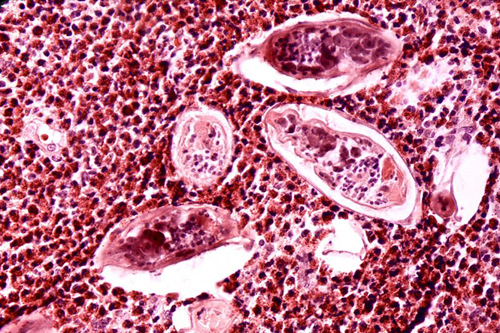
Schistosomiasis regularly infects children
Scientists showed that in fact, infection rates are high among pre-school children. This may be because they often accompany their mothers to rivers and wells.
Symptoms of the disease – which can include impaired memory and thought as well as damage to internal organs and stunted growth – are not always obvious.
The study found that a common snail fever drug, known as praziquantel, which is regularly given to older children and adults, can safely cure the infection in infants. The treatment is cheap and effective, curing infection and stopping progress of disease in a single dose.
Researchers from the University of Edinburgh carried out studies in Zimbabwe and their results were combined with work by other teams in Mali, Sudan, Egypt, Niger and Uganda. In a recent World Health Organisation report, the teams recommended that infants be included in treatment programmes, and their work is informing public health policy.
According to the WHO, snail fever affects 230 million people each year, most of whom are African. Some 33.5 million people were treated for the disease in 2010. Children are especially vulnerable because they make frequent contact with infected water.
Dr Francisca Mutapi, of the University of Edinburgh’s School of Biological Sciences, who took part in the study, said: “Snail fever is a widespread disease of major health consequence in young children. Our study shows that infants are especially vulnerable to infection and should be included in public health treatment programmes.”